Background: Cannabis use has grown in popularity, with the possible therapeutic advantages being widely debated, one of which is in Sickle Cell Crisis (SCC). With increasing surveys reporting overlapping use of recreational and medicinal cannabis and high addiction potential, the aim of this nationwide study is to investigate the relationship between cannabis use disorder (CUD) in SCC patients.
Methods: Using ICD-10 codes, the National Inpatient Sample-2020 was utilized to identify adult (>18 years) hospitalized patients due to SCD with and without crisis and further divided into patients with SCC with CUD (SCC+CUD+) and patients with SCC without CUD (SCC+CUD-). The prevalence of CUD in SCC and Major Adverse Cardiac Events [MACE, Acute Myocardial Infarction (AMI); Atrial Fibrillation (AFib) and cardiac arrest] were the primary outcomes; other associated comorbidities, Length of Stay (LOS), and hospitalization costs were secondary outcomes. After examining the baseline features on descriptive analysis, to compare the variables, Pearson's chi-squared test and Mann- Whitney U test were used to compare categorical and continuous data, respectively. Multivariable analyses were performed, controlling covariates, to assess the odds of MACE in the CUD+ vs. CUD- cohort.
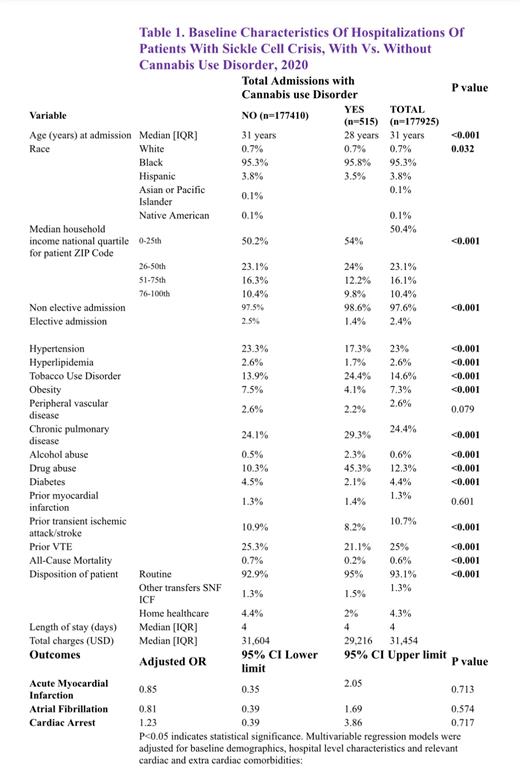
Results: Out of a total of 77,610 SCC adult hospitalizations, 4,535 (5.8%, p<0.001) had CUD. The median age of hospitalization for the CUD+ cohort was lower (28 years) than for the CUD- cohort (31 years). They were often of black ethnicity (95.8% vs. 95.3%, p=0.03), Medicaid enrollees (55.3% vs. 46.3%, p<0.001), and were hospitalized as non-electively (98.6% vs. 97.5%, p<0.001) to urban teaching hospitals (87% vs. 85.5%, p<0.001) in the Southern (47.7% vs. 53.7%, p<0.001) region. Chronic Pulmonary diseases (29.3% vs. 24.1%, p<0.001), prior venous thromboembolism (21.1% vs. 25.3%, p<0.001), hypertension (17.3% vs. 23.3%, p<0.001) and depression (16.3% vs 13.5%, p<0.001) were the majorly associated comorbidities in both (SCC+CUD+) and (SCC+CUD-) cohorts. On analysis of MACE in SCD patients with crisis; AMI (0.6% vs 0.7%, p=0.28), AFib (0.3% for both, p<0.001), cardiac arrest (0.3% for both, p = 0.89) were comparable in both SCC cohorts with and without CUD, suggesting no significant difference in MACE between these patient groups except for AFib. However, after adjusting for confounders, on multivariable analysis, none of the MACE (AMI: OR=0.85, CI= 0.35-2.05, p=0.71; AFib: OR=0.81, CI= 0.39-1.69, p= 0.57; cardiac arrest: OR = 1.23, CI= 0.39-3.86, p= 0.71) were found to be significant, p>0.05 for all. In (SCC+CUD+) and (SCC+CUD-) patients, there was no difference observed in LOS (4 days in both) and hospitalization costs (USD 29,216 vs. USD 31,604).
Conclusion: Our study evaluated the prevalence and association between CUD and its cardiovascular effects during SCC, bringing light on an essential and understudied association in SCC patients while adjusting for other major concomitant mixed substance abuses like tobacco and alcohol. The observed disparities in MACE require further exploration via prospective research to better understand the possible recreational and therapeutic implications of cannabis use in patients with SCC.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal